Can Digital Health Help Stop the Next Epidemic?
"Can Digital Health Help Stop the Next Epidemic?." CSIS Commission on Strengthening America's Health Security, Center for Strategic and International Studies, October 11, 2019. Accessed October 01, 2025. https://healthsecurity.csis.org/articles/can-digital-health-help-stop-the-next-epidemic/
The Issue
Timely and accurate information to assess disease burdens, track emerging outbreaks, and support disease prevention and control measures is essential in epidemic response. When optimized, the convergence of digital technologies and new data models with health systems, also known as “digital health,” can help ensure the necessary data and information are available in the right place, at the right time, and to the right people. This paper recommends a focused five-year U.S. initiative to pilot replicable U.S. models for scaling digital health within U.S. epidemic preparedness and response efforts in two to three partner countries.
Overview
Timely and accurate information to assess disease burdens, track emerging outbreaks, and support disease prevention and control measures is essential in epidemic response. Over the past decade, low- and middle-income countries (LMICs) have increasingly transitioned from paper-based to digital information systems and are utilizing new technologies to collect data. This increasing uptake of digital technologies and data tools to support global health security allows countries to make more accurate and timely decisions for preventing, detecting, and responding to outbreaks. When optimized, the convergence of digital technologies and new data models with health systems, also known as “digital health,” can help ensure the necessary data and information are available in the right place, at the right time, and to the right people.[^1]
Over the last five years, the U.S. government has made a number of smart investments in a variety of digital tools and approaches and has worked to strengthen the capacity of local partners to utilize these tools.[^2] While clear successes have resulted from these initial investments, significant challenges remain:
- Many health information systems are siloed and capture duplicate data, putting significant strain on health workers who collect, manage, and use this information.
- Health information systems are not always interoperable—they cannot always “talk” to one another—which hinders evidence-based decision-making.
- The capacity of stakeholders to design, manage, and support digital health systems, as well as effectively use data, is critically needed in many LMICs.
- Many countries lack the necessary governance structures, policies, and coherent national plans to support the utilization of data to inform decisions and actions in epidemic response.
- The U.S. government has not sufficiently leveraged the potential of the U.S. technology sector to advance digital health and global health security goals.
There is understandable skepticism about the successful application and utilization of digital technologies in fragile and disordered settings. This proposed initiative would be designed to prove that, with targeted strategic investments, it is possible to rectify these persistent challenges and realize the full potential of digital technologies in LMICs. We recommend that the U.S. government launch an initiative that will:
- Expand the use of interoperable data systems;
- Strengthen governance and national plans to share data and scale up proven tools under the direction of country health authorities;
- Build capacity and leadership to interpret data and act upon it; and
- Utilize new financing mechanisms to better leverage the potential of the U.S. technology sector.
This initiative will require a strategic, focused effort across all U.S. agencies engaged in global epidemic preparedness and response, and a modest investment—we recommend $20 million each year—as a component of Global Health Security Agenda investments across the CDC, USAID, and Department of Defense. New financing mechanisms, such as the U.S. Development Finance Corporation (USDFC), offer an important opportunity to create new partnerships and unlock private capital to advance digital health and epidemic preparedness.
Such an initiative will demonstrate proof-of-concept for a higher standard of U.S. coordination and engagement to strengthen digital health and generate learnings that will benefit other global health security efforts in the next decade and beyond.
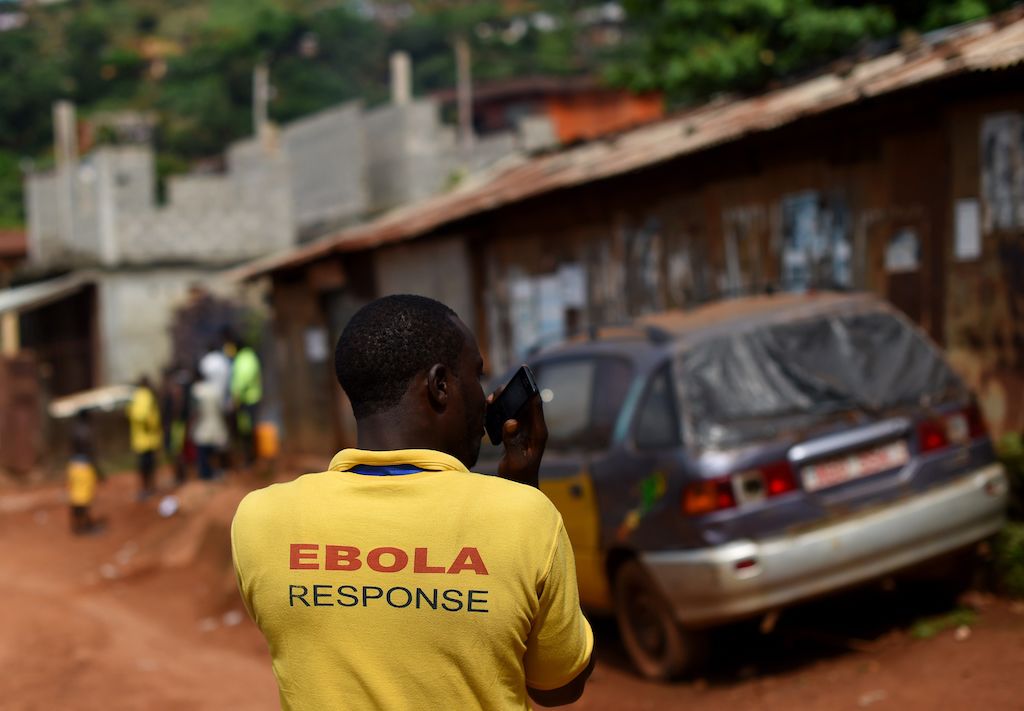
Case Study: West Africa Ebola Outbreak
When the Ebola outbreak hit West Africa in late 2013, the world was caught unprepared. Quality data is the foundation of any outbreak response effort. But at the outbreak’s peak, stakeholders involved in the international response effort lacked digitized information on the location of cases and accurate maps for logistics, population estimates, treatment centers, community outreach, and social mobilization efforts, as well as the location of supplies. Accurate data on outbreak hotspots and individual data on sick persons and contacts was not readily available. Data collection practices differed between field and research epidemiologists, leading to confusing and inaccurate forecasting. Furthermore, international stakeholders involved in various aspects of the response had no common platform to share data across sectors, locations, and authorities.
USAID’s administrator at the time convened a group within USAID to examine the root causes of the “fog of information” hampering the response effort.[^3] The group determined that a variety of data and digital systems impediments led to these conditions, including health information system weaknesses, limitations on data sharing due to privacy concerns, poor utilization of non-digitized data in modeling and forecasting, and gaps in digital connectivity.
This example points to the impact that data and digitization—or the absence of it—can have in epidemic response. In fact, USAID’s experience in West Africa ultimately led to a much greater emphasis on digital health within its current global health efforts.[^4] However, the learning curve in this rapidly evolving area of global health is steep, and several elements must be in place to realize the full benefit of data and digitization in preventing, detecting, and responding to epidemics.
Persistent Challenges in Digital Health
Digitization alone does not strengthen health outcomes.
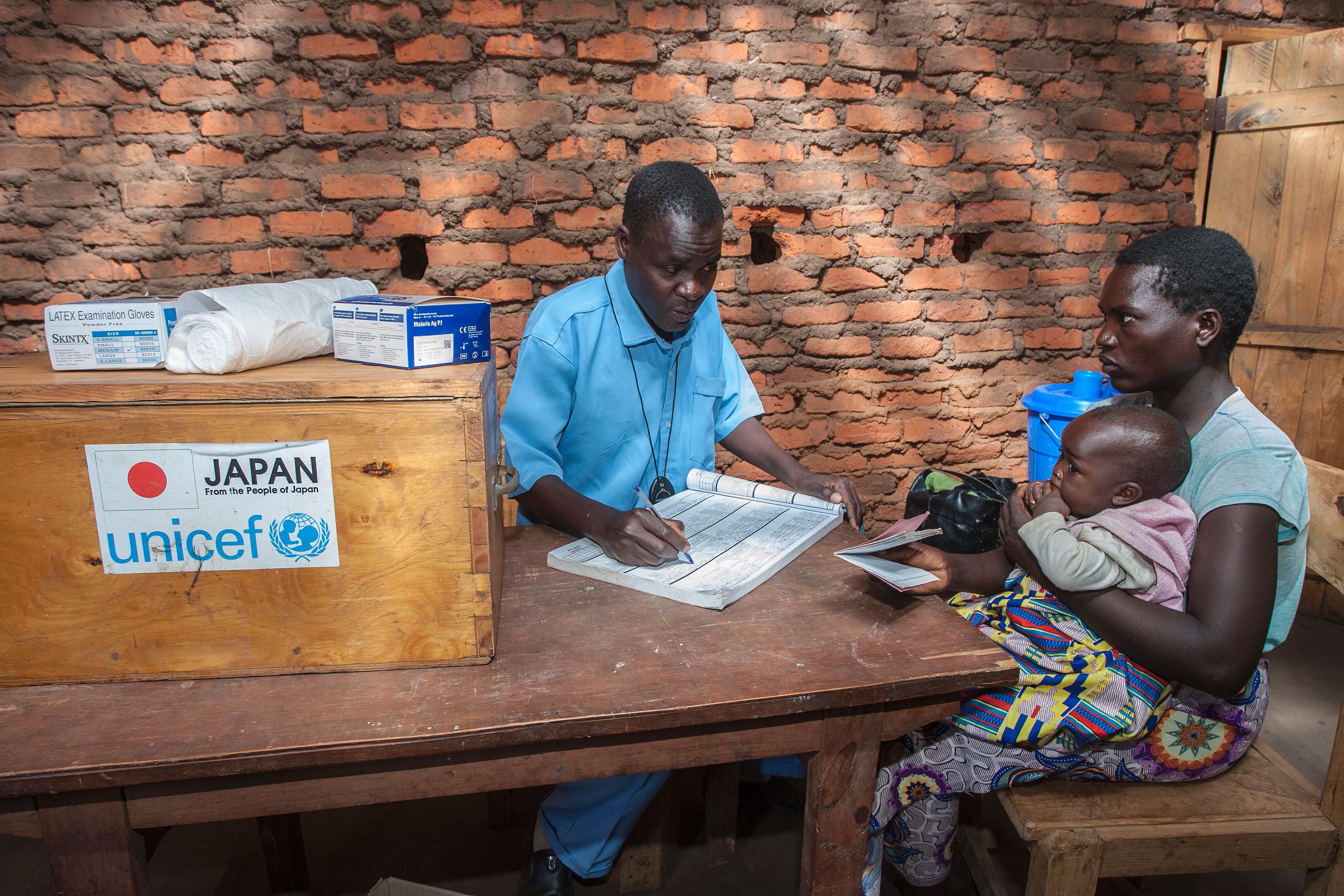
Over the past decade, countries have increasingly transitioned from paper-based to digital information systems and have gained new capabilities and insights by engaging in the corresponding data. Various open-source and commercial software products have been developed to digitally capture and visualize improved data, including health service information management, health worker location, client medical records, and supply chain updates. However, not all efforts to digitize data have resulted in better information for decision-making. Many examples exist of technologies that overpromised and underdelivered in real world settings. Additionally, many data capture tools have been deployed in a fragmented and duplicative way, increasing the burden on public health officials and decreasing efficiencies in the health system. Efforts to enhance data quality and analysis alongside digitization efforts are essential for effective data use.
The reduction of data errors can be simplified by investing in interoperability—defined as the ability of systems to share and exchange data using open standards and software connections. When accompanied by corresponding investments in country health systems and training of key users of this data across sectors, interoperability has proven to increase data exchange among various health systems and, as a result, strengthen health infrastructure and access to appropriate health interventions.[^5]
Additionally, while there has been great advancement in new digital tools and approaches, it has not been matched by adequate capacity building of local and regional stakeholders. Without significantly increased investment in training, uptake of digital tools will be slow, and they may be used incorrectly.
Furthermore, even in settings where digital tools exist, if there is not a strong system to analyze and organize the data to coordinate a multisectoral response, overall efforts will be hampered. Where they have been established, emergency operating centers (EOCs) dramatically improve a country’s preparedness and response capabilities. Built on a culture of data use, EOCs bring surveillance data and other information from a variety of sources into a central decision-making authority. Stakeholders with the capacity to interpret data, governed by standard operating procedures, recognize signals of health threats and act quickly to contain them. Often operating under a country’s prime minister or minister of health, EOCs consolidate data and decision-making in a central authority and implement solutions across sectors within a country. Where they are in place, EOCs provide a central node of leadership critical to preventing, detecting, and responding to epidemics. Where they do not exist, or are not yet up to the task, health security efforts are hampered.
Disincentives to data sharing prevent collaboration when it is most needed.
Equally as important to the tools and technologies themselves are the governance structures and policies supporting the tools and people who use them. Good digital and data governance helps support a dynamic policy and regulatory environment, positioning enabling structures to support the use of data to inform the decisions and actions required for epidemic response at all levels of the health system. National digital health plans help ensure that proven and scalable technologies are adopted under the direction of capable national health authorities and complement, rather than compete with, the capabilities of existing health information systems.[^6],[^7]
Governance of information flows—data ownership, access, standards, privacy, security, and sharing—are essential elements of an efficient epidemic surveillance and control system. In data sharing, for example, governance around sharing data is often a barrier to effective utilization of data and digital health tools in the context of epidemic preparedness and response. As was seen in the West Africa Ebola outbreak example, in the absence of strong digital and data governance structures and standards, health authorities will struggle to reconcile disparate data systems and share this data with actors involved in epidemic response. Furthermore, this information, when reported to UN agencies, needs to be immediately shared with the appropriate actors in the global community for action; any delays in doing so hamper response efforts.
Rapid sharing of data is critical in detection and response to outbreaks, yet national policies that prohibit data sharing due to concerns about privacy and sovereignty, as well as political and economic concerns, can limit the exchange of information even in circumstances when it is most needed. Urgency around the need for information must be balanced with the growing complexity and importance of protecting the privacy of patients, communities, and health workers.
Digital and data governance is, at its essence, a capacity and political issue, not a technological one. Aligning and streamlining decision-making structures is a good start, but the health workers at the core of digital and data governance structures must also have the information, capacity, and authority to function and lead. Coupling this capacity strengthening with the institutionalization of strong digital health governance structures, processes, and norms through legislative bodies and executive agencies. It will not only encourage sustainability that can weather changes in leadership but also build a domestic financial base for digital and data activities and facilitate the institutionalization of data use. The U.S. government should work with national government partners to develop the structures that govern digital and data in a fashion that aligns current health, data, and digital infrastructures and which can iterate and adjust to address how diseases and public health needs evolve moving forward.
Data access and security policies need to be well defined to be effective. Data-sharing agreements can determine the terms for data sharing in advance, should it be needed for epidemic response. These agreements, however, can be difficult to negotiate. Governance structures define the way duty bearers in different jurisdictions and departments will access, communicate, and share information with one another, while maintaining sovereignty and ensuring appropriate privacy protections. Therefore, these agreements must address the complex legal and procedural standards of each of the entities involved.
Another consideration in data governance is the need to limit the intentional misuse of data through strengthened cybersecurity measures. The potential for malicious actors to deliberately inject chaos in disease response efforts through cyberattacks or misinformation campaigns presents a challenge to international efforts to digitize health systems and facilitate data sharing. Indeed, these threats are a growing concern, and safeguards must be in place to ensure that data can be shared and used safely.
A more coordinated U.S. effort is needed.
Enabled by technological advances and building on the lessons learned since the West Africa Ebola outbreak, digital health has emerged as a key strategy across U.S. agencies and departments engaged in epidemic preparedness. Enhanced digital health capabilities support the broad mandates and strategic goals of agencies like the CDC, USAID, and the DOD and can enable them to achieve their broader global health security objectives.
Enabled by technological advances and building on the lessons learned since the West Africa Ebola outbreak, digital health has emerged as a key strategy across U.S. agencies and departments engaged in epidemic preparedness.
With a focus on zoonotic diseases, workforce development, disease surveillance, and antimicrobial resistance, USAID and the CDC use digital systems in their collaboration with national and community stakeholders to monitor threats with epidemic potential. USAID also invests in research and development (R&D) for new digital tools through Grand Challenge financing.[^8] As the technical implementation lead for U.S. health security and the Global Health Security Agenda, the CDC combats health threats using multiple interoperable digital health information platforms, including supporting critical surveillance and laboratory systems, EOC training and development, diagnostics, health workforce development, and antimicrobial resistance measures and stewardship. Through the enhancement of R&D, biosecurity, and biosurveillance, the DOD invests in digital systems to prevent and respond to outbreaks of infectious disease that may threaten international and domestic stability.
While many U.S. agencies are implementing or supporting groundbreaking digital health initiatives, coordination between these initiatives must be resourced and mandated within each country context under the direction of the U.S. embassy. As prescribed in the 2019 United States Government Global Health Security Strategy, the CDC, USAID, and their implementing partners have begun to convene quarterly in six partner countries to share lessons learned and coordinate efforts.[^9] A consolidated report to the NSC captures lessons learned across the partners. This practice should be encouraged and broadened to additional countries.
Furthermore, standards and common definitions do not exist across the U.S. government, or even among the agencies that collaborate around epidemic prevention, detection, and response—a fix that would vastly improve the ability of U.S. entities to build upon one another. Lastly, due to silos and stovepiping, there is a lack of sharing and knowledge management around different tools, particularly between the U.S. agencies with global health mandates (the CDC and USAID) and the DOD. Without coordination, there is a risk of developing different and potentially duplicative systems.
Contributions from the private sector are underleveraged.
Advancements in digital tools have largely been driven by the private sector, yet the sustained engagement of industry to advance global health goals is underutilized. Private companies bring specialized expertise to the development of innovations for digital health but often lack needed access to user interfaces and insights on the workings of public health systems to design the best tools. The full potential to utilize their capacities, in-kind contributions, and resources is limited without a more effective partnership between the private sector and governments, donors, public health authorities, and other global health players. Furthermore, failure to effectively engage industry players means private-sector capital to advance digital health innovation is being left on the table.
There is tremendous unrealized potential to engage the U.S. technology sector in U.S. preparedness and response efforts. U.S. companies have increasingly high standards for data protection and privacy, and many have navigated these challenges in a complex and changing regulatory and normative environment within the United States. Engaging U.S. companies to advance digital tools around the globe could offer products and innovations that more fully address countries’ concerns about data protection and privacy and unlock new capabilities, tools, and approaches for data analysis, interoperability, and digital payment.
Building on Recent Progress in Digital Health
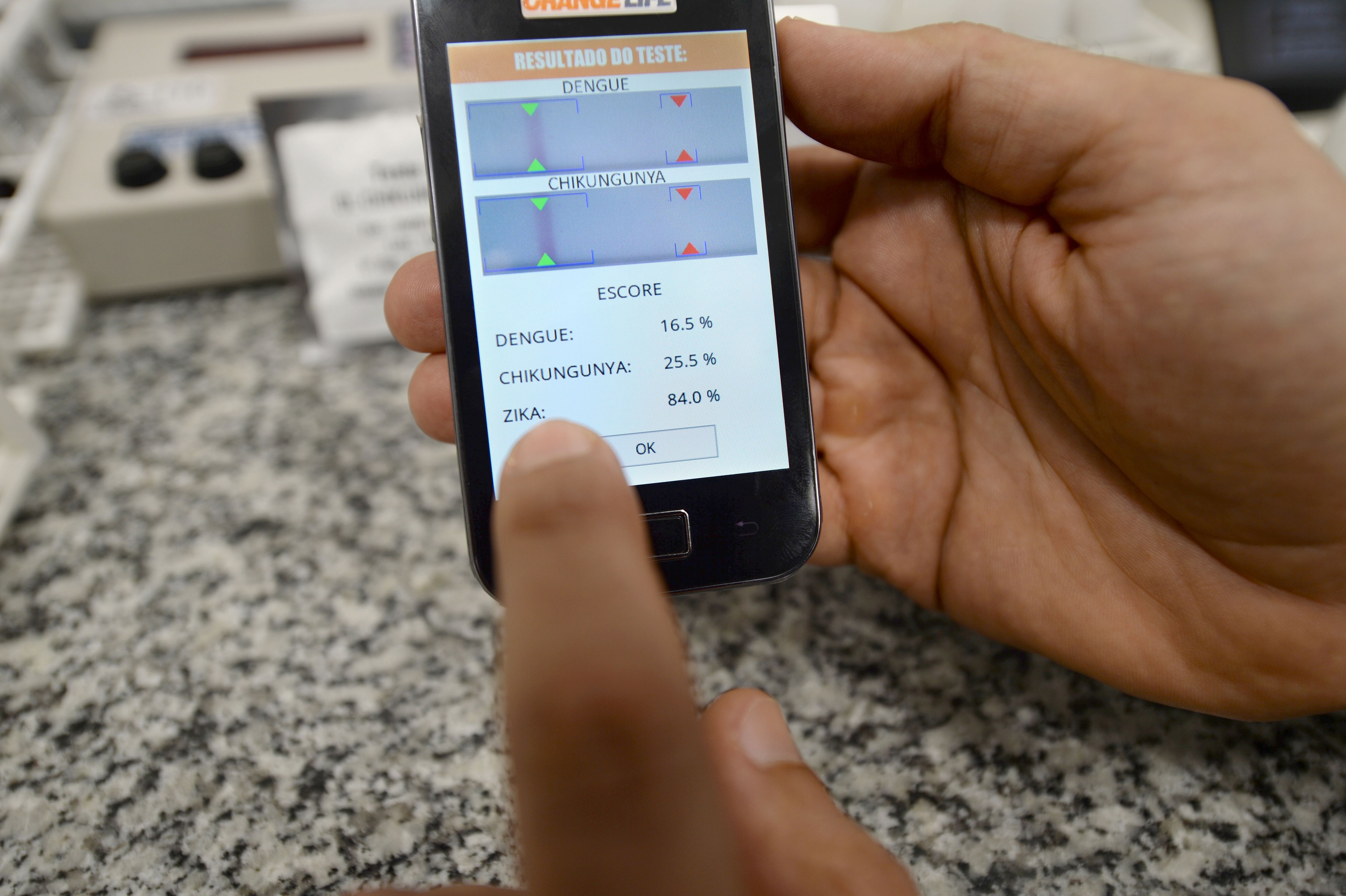
Harnessing the capabilities of digital technologies, big data, machine learning, and artificial intelligence (AI) could help strengthen prevention measures by predicting potential future epidemic outbreaks and targeting communications for behavior change. With this information, officials would have the capability to strengthen efforts to prevent outbreaks before they occur.
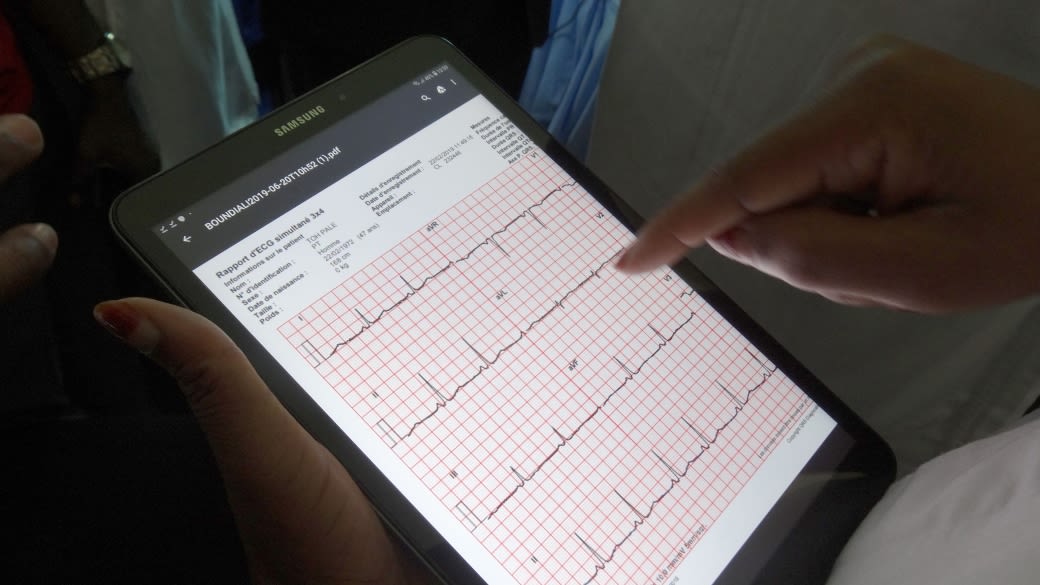
More timely and accurate collection and sharing of high-quality data at all levels, through enhanced surveillance and laboratory tools, could help rapidly detect cases before outbreaks become epidemics. Interoperability, designed and implemented effectively, could increase the speed and accuracy of confirming suspected cases. Harnessing mobile technology to enable faster collection and sharing of data accelerates early detection even at the front line. Easier and more efficient data flow in times of crisis, such as using digital tools to track and manage commodity supply chains in real time, speed response and can spell the difference between an epidemic and a pandemic.
Examples of Impact
- Artificial Intelligence in Medical Epidemiology (AIME) is an AI-enabled platform supported by USAID that uses a variety of physical and environmental factors to predict future outbreaks of diseases like Zika and dengue months in advance. This technology has been used in Rio de Janeiro, Singapore, and Malaysia, leading the countries to accurately predict dengue outbreaks within 400 meters and up to three months in advance, with 88.7 percent accuracy.[^10]
- The electronic Integrated Disease Surveillance and Response (eIDSR) system, supported by USAID and other donors, is used to improve and customize the flow of information within health programs, building on the existing DHIS2 platforms in many countries. In Sierra Leone and Tanzania, all districts electronically report their IDSR data to the national level, reducing the number of data entry errors by half and capturing and verifying data 60 percent faster than the paper-based IDSR system.[^11]
- In Vietnam, a CDC electronic surveillance platform is now functional for 44 communicable diseases and syndromes in all 63 provinces and 711 districts, allowing real-time reporting and information sharing between the clinical and preventive medicine sectors.[^12]
Some of these benefits are already being realized. In the last five years, investments in data and digitization have contributed substantially to increasing the capabilities of countries to improve epidemic preparedness and response. The U.S. government should maintain and build upon these recent successes to realize the full potential of digital health in preventing, detecting, and responding to outbreaks.
Interoperable systems will strengthen preparedness and speed detection and response.
Truly harnessing the potential of digital health to help prevent, detect, and respond to global health threats requires digital health information systems that enable exchange of data and information. Facilitating interoperability improves data quality and allows users more information at their fingertips, enabling more efficient strategic decisions. For example, interoperability could allow a lab system to automatically share test results of a suspected case back to an electronic patient record, seamlessly connecting the results with the patient. Health providers could pull up the health record, review the lab results, and determine the best treatment—a practice taken for granted in high-income settings but absent in many countries facing outbreaks.
U.S.-supported efforts to create interoperable systems are nascent but encouraging. For example, a study conducted by the Cross-Border Health Integrated Partnership Project identified the need for standardized, interoperable health management information systems and an accompanying policy framework to facilitate data sharing across facilities, districts, counties, and countries.[^13] After two years of assessments across five Eastern African Community (EAC) partner states, the project determined that interoperable systems supported by robust policy are critical to effectively achieving sustainable cross-border service delivery for vulnerable populations in East Africa.[^14] As a result, USAID initiated an East Africa cross-border health service and referral program that has been approved as a priority investment by all six presidents of the EAC countries.
Enhanced digital and data governance will break down barriers to coordination between authorities.
Having strong digital and data governance policies and practices in place in advance of an epidemic can dramatically speed health authorities’ ability to detect and respond to health threats.[^15] This includes elements such as data-sharing agreements between countries and between public and private partners within countries, establishing common standards to support sustainable interoperability of health information systems, and aligning local agencies that govern digital health, eGovernment, data regulatory functions, and public administration in support of ministries of health. Furthermore, the impact of digital health technologies is further enhanced under national digital health plans—led by country health authorities and supported by donors and partners—that ensure proven and adaptable solutions can be scaled and that local decisionmakers have the capacity to use them.
Building on the recent Ebola outbreaks and the efforts of its emergency operations center (EOC), the Democratic Republic of the Congo’s (DRC) Ministry of Health recently launched the Agence Nationale d’Ingénierie Clinique d’Information et d’Informatique de Santé (ANICiiS)—a new national agency for clinical information and health informatics. With a mission to improve management of the health care system, quality of care, and accessibility of services, the ANICiiS is the country’s first dedicated digital health agency.
Sustaining and increasing U.S. government support for similar interventions, such as the Africa CDC’s program to design and implement a continental data-sharing platform for African Union member states and providing informatics training through its Regional Coordination Centers (RCCs), is important to the integration of digital and data governance and fostering coordination between governments, regional bodies, and key private-sector partners.
Digital and data governance is essential for supporting emergency response coordination, as well as accelerating progress of routine health programs. We are just now beginning to unlock the capabilities of digitally- and analogically-produced data to support health workers, donors, policymakers, and other partners in informing health programming and improving health outcomes. The next decade will not only see accelerated innovation in emerging technologies but is also expected be an era of improvement in more traditional forms of data collection, management, and utilization. As these advances progress, connecting enhanced data systems and tools with strong digital and data governance decision-making structures and effective policies will be a critical element to the success of all health programs.
Stronger alignment across U.S. agencies will result in greater health impact.
Stronger and more strategic alignment across U.S. agencies will improve how digital technologies augment and support global health security efforts. Perhaps the most visible example of interagency coordination in data systems and use in U.S. programs is the President’s Emergency Plan for AIDS Relief (PEPFAR). PEPFAR’s goal to reach epidemic control necessitates precision data, down to the service delivery level, to drive its outcomes. Through its implementing agencies, PEFAR supports laboratory information systems, electronic medical record information systems, and HIV case-based surveillance systems in 30 countries to automate patient-level reporting and aggregate data. It also supports applied informatics capacity development and training programs aimed at developing individual and organizational capacities of counterpart ministries of health and local partners. PEPFAR’s considerable investment in data, digital tools, and innovations alongside health programming demonstrates the impact that can be achieved with a focused digital health effort implemented across U.S. agencies. While some of PEPFAR’s data systems are isolated and dedicated to reporting primarily within the PEPFAR structure, the approach is nonetheless a helpful case study in interagency coordination.
Other promising examples of alignment within the U.S. government also exist. Through the USAID-funded Infectious Disease Detection and Surveillance project (IDDS), there have been opportunities to streamline U.S. agency support to digital health activities in priority countries.[^16] The project focuses on increasing the detection and surveillance of infectious diseases and antimicrobial resistance in 16 countries. From project initiation to implementation, USAID has ensured strong connection between other U.S. agency partners supporting global health security, such as the CDC. Open communication and coordination are allowing a more streamlined approach at the country level, where regular meetings are held between program staff from USAID, the CDC, the IDDS, and CDC’s Global Health Security Agenda partners.
Internationally, U.S. agencies have joined with other governments, foundations, and the private sector to develop the Principles of Donor Alignment for Digital Health.[^17] These principles reorient stakeholders, including U.S. agencies, to pursue an integrated approach to strengthening digital health systems in countries and align investments to country digital health strategies. Additionally, new WHO guidance on digital interventions for health system strengthening and its Global Strategy on Digital Health 2020-2024, as well as the International Standards Organization’s standards for health informatics, create common terms and approaches for digital health, which are lacking across U.S. agencies. Aligning with these global frameworks may help U.S. agencies to more coherently approach and plan for investments in digital health among themselves and interface more effectively with other international actors involved in emergency preparedness and response.
Effective engagement of the private sector will bring new digital tools and capacities.
When effectively mobilized, the private sector catalyzes critical investments, as well as resources, expertise, and know-how, for digital health information systems. Private-sector engagement has enabled many recent innovations that are making a difference in preparedness and response.
Private-Sector Contributions to Emergency Preparedness and Response
- In Guinea, a consortium of partners, including the Guinean Ministry of Health and USAID, developed the use of the CommCare contact tracing tool to gather and share critical case data. An online dashboard provided by Tableau, a Seattle-based technology company, was used to visualize contact tracing data in real time. The app collected nearly 30,000 contact tracing forms across five of the eight prefectures in Guinea, which led to a reduction of delays and human error and increased reliability, data verification, and contact tracer accountability.
- Qlik, a data analytics company and member of the Global Health Security Agenda Private Sector Roundtable, created an online tool which draws from information contained in countries’ Joint External Evaluations, as well as its own data, to create dashboards that showcase countries’ health security capabilities.
Innovation in the private sector holds tremendous potential for the future of health security. Cutting-edge AI applications and machine learning can be applied to rapidly identify early outbreak signals and accelerate response time, and companies that specialize in data analytics and visualization are designing new tools so health authorities can better use data for decision-making. To ensure evidence-based health information reaches communities around the world, there is a tremendous opportunity—and urgent need—to partner with social media companies to combat harmful misinformation and promote health messages. Digital applications could also help address operational challenges in health delivery. For example, missed payments to health workers in both of the previous Ebola outbreak in West Africa and the current outbreak in the DRC have been hugely problematic.[^18] Fintech applications and mobile banking that enable direct payment of health workers prevent corruption and motivate those on the front lines of an epidemic.[^19]
During the Ebola outbreak, private-sector companies contributed financing and scale up of digitized health interventions for logistics and supply chain and data management.[^20] Since then, many partnerships with industry have been formed through the Global Health Security Agenda Private Sector Roundtable, a forum for linking private-sector companies with global actors involved in strengthening health security.[^21] While these collaborations are a promising signal, engagement of a broader set of industry partners would strongly benefit from a more powerful partnership mechanism.
Sustained government investment and incentives to secure ongoing commitment are key to engaging the private sector. U.S. technology companies have led in the digital and data revolution and could be a tremendous asset to U.S. efforts to enhance epidemic preparedness through data and digital innovation. Partnership mechanisms to draw in their skills and capacities could be a game-changer.

Authorized in 2018, the U.S. International Development Finance Corporation (USDFC) will soon open its doors.[^22] This new entity, designed to draw in new private-sector partners, is authorized to participate in equity investments; issue direct loans and guaranties; provide political risk insurance and fund first loss guarantees; and provide limited grant and technical assistance to unlock larger investments. By creating new models of partnership and financing, the USDFC could bring a range of new industry partners to the table to advance health innovations, from biomedical products to digital health technologies. This new mechanism should be strongly considered for strategically and purposefully deploying incentives that bring industry to the table.
Addressing the Gap
Despite recent successes, skepticism persists regarding the application and utilization of digital technologies in fragile and disordered settings. This proposed initiative would be designed to prove that with targeted strategic investments it is possible to rectify these persistent challenges and realize the full potential of digital technologies in LMICs.
We propose a focused five-year U.S. initiative to pilot replicable U.S. models for scaling digital health within U.S. epidemic preparedness and response efforts in two to three partner countries. This effort should focus on:
- Designing and scaling interoperable digital health information systems;
- Building capacity in LMICs to collect data digitally and use it for decision-making;
- Strengthening digital and data governance; and
- Leveraging the potential of the private technology sector in the United States;
Several countries in West and East Africa, where regional efforts to strengthen digital health infrastructure have driven rapid progress, could be good candidates for such an initiative. Senegal and Tanzania, for example, have shown strong leadership within their respective regions in adopting and scaling up digital health approaches.[^23],[^24] Countries in Southeast Asia—like Vietnam, where a plethora of U.S. projects are rapidly transforming the digital health landscape—should also be considered.
Given the centrality of data and information in preventing, detecting, and responding to outbreaks, positioning this initiative within U.S. investments in the Global Health Security Agenda will offer the ideal conditions to observe and refine models for strengthening digital health solutions in LMICs. Building on current programming within the CDC, USAID, and the DOD, this initiative should incentivize the use of digital health tools and expand technical assistance for data use. Development and deployment of interoperable health information systems that can efficiently collect health data and provide real-time analytic insights will accelerate decisions and action, improve the quality of services, and empower local authorities to drive the response effort.
To facilitate rapid collaboration with key actors, U.S. agencies should also support efforts to strengthen data governance and negotiate preparedness protocols with key actors such as local leaders, policymakers, regional and national governance bodies, civil society, academia and research organizations, and the private sector to increase telecommunications networks and data sharing in advance of outbreaks.
The U.S. government is in a strong position to leverage its resources and build on proven strategies to meet existing gaps that are inhibiting digital technologies in LMICs.
The U.S. government is in a strong position to leverage its resources and build on proven strategies to meet existing gaps that are inhibiting digital technologies in LMICs. Applying best practices and lessons learned over the past decade, the U.S. government is uniquely poised to scale replicable approaches in digital technologies, apply innovative solutions, and harness strategic partnerships to help key partner countries.
This initiative will demonstrate proof-of-concept for a higher standard of U.S. coordination and engagement to strengthen digital health and generate knowledge that will benefit other digital health programming across the U.S. government. It will form the evidence base for increased investments in digital health within the context of epidemic preparedness and response, as well as global health efforts more broadly, in the decades to come. We recommend that the initiative be coordinated with and complement related programs within the CDC, USAID, and the DOD working to expand the use of data and digital tools.
We estimate that an investment of $20 million per year, embedded within a larger investment in the Global Health Security Agenda, would enable demonstrated impact of digital technologies in strengthening health security and preparedness capacities. We recommend that these resources—which would be distributed within budget lines for health security operations of the CDC, USAID, and the DOD—be centrally coordinated and dedicated to the purpose of developing interoperable digital health information systems and strengthening data governance in the selected partner countries.
In addition to these dedicated funds, we encourage the CDC, USAID and the DOD to consider where scaling up digital health efforts will advance progress toward global health security goals in each agency’s priority countries. Sustained investment in digital health across agencies will drive the development, integration, and adoption of digital health technologies and fuel several activity streams, from policy support, to tool development, to adoption and implementation. Investments in digital health for global health security will also strengthen other health domains such as malaria, measles, and HIV/AIDS, producing lessons for epidemic response and global health at large.
Alongside this focused effort, we also recommend that the USDFC invest in digital health infrastructure in order to catalyze partnerships with the private sector that will more fully leverage resources and expertise to advance health security. The USDFC has the potential to create new and innovative public-private partnerships to advance U.S. development objectives. Where this remit overlaps with U.S. interests in strengthening the digital health capacities of low- and middle-income countries, there is a clear business case—and promising investment opportunity—for investing in health data infrastructure to advance global health security. This new mechanism will bring new capital to the table and enable the capacities and resources of the private sector to be better utilized.
Conclusion
The U.S. government has an opportunity to use digital health tools to significantly enhance global capacity to prevent, detect, and respond to threats to global health security. This can be achieved through the dedicated development of interoperable digital health information systems, strengthened data governance, and capacity building, as well as efforts to strengthen country coordination and leadership, such as through EOCs. With coordinated and strategic investment across departments and programs, the U.S. government has an opportunity to prove what is possible in leveraging digital tools to prevent, detect, and respond to infectious disease outbreaks.
A more coordinated and focused U.S. effort will strengthen U.S. leadership in global health security and drive innovations in digital health through engaging public- and private-sector partners at home and abroad. Creating this enabling environment to fully capitalize on the promise of digital health innovation will help protect America’s health security while strengthening global capacities to address health security threats wherever they may occur.
This Brief was written by PATH as part of its collaboration with the CSIS Commission on Strengthening America’s Health Security. PATH is a global organization that works to accelerate health equity by bringing together public institutions, businesses, social enterprises, and investors to solve the world’s most pressing health challenges. With expertise in science, health, economics, technology, advocacy, and dozens of other specialties, PATH develops and scales solutions—including vaccines, drugs, devices, diagnostics, and innovative approaches to strengthening health systems worldwide.
This brief is a product of the CSIS Commission on Strengthening America’s Health Security, generously supported by the Bill & Melinda Gates Foundation.
CSIS Briefs are produced by the Center for Strategic and International Studies (CSIS), a private, tax-exempt institution focusing on international public policy issues. Its research is nonpartisan and nonproprietary. CSIS does not take specific policy positions. Accordingly, all views, positions, and conclusions expressed in this publication should be understood to be solely those of the author(s).
© 2019 by the Center for Strategic and International Studies. All rights reserved.
[1] World Health Organization (WHO), Global Strategy on Digital Health 2020-2024 (Geneva: March 2019), https://extranet.who.int/dataform/upload/surveys/183439/files/Draft%20Global%20Strategy%20on%20Digital%20Health.pdf.
[2] “Global Health News - Digital Health,” USAID, https://www.usaid.gov/global-health/global-health-newsletter/digital-health.
[3] USAID, Fighting Ebola with Information: Learning from the Use of Data, Information, and Digital Technologies in the West Africa Ebola Outbreak Response (Washington, DC: 2016), https://www.usaid.gov/sites/default/files/documents/15396/FightingEbolaWithInformation.pdf.
[4] Ibid.
[5] WHO and International Telecommunication Union, National eHealth Strategy Toolkit (Geneva: WHO, 2012), https://www.itu.int/dms_pub/itu-d/opb/str/D-STR-E_HEALTH.05-2012-PDF-E.pdf.
[6] Broadband Commission for Sustainable Development Working Group on Digital Health, The Promise of Digital Health: Addressing Non-communicable Diseases to Accelerate Universal Health Coverage in LMICs (Geneva: September 2018), https://broadbandcommission.org/Documents/publications/DigitalHealthReport2018.pdf.
[7] Sophie Edwards, “Tanzania’s new digital health road map has the government ‘in the driver’s seat’,” Devex, December 16, 2016, https://www.devex.com/news/tanzania-s-new-digital-health-road-map-has-the-government-in-the-driver-s-seat-89324.
[8] “Innovations,” USAID, http://www.ebolagrandchallenge.net/innovations-3.
[9] White House, United States Government Global Health Security Strategy (Washington, DC: 2019), https://www.whitehouse.gov/wp-content/uploads/2019/05/GHSS.pdf.
[10] USAID, Rockefeller Foundation, Bill & Melinda Gates Foundation, Artificial Intelligence in Global Health: Defining a Collective Path Forward (Washington, DC: April 2019), https://www.usaid.gov/sites/default/files/documents/1864/AI-in-Global-Health_webFinal_508.pdf; “Artificial Intelligence in Medical Epidemiology (AIME),” One Young World, https://www.oneyoungworld.com/ambassador-projects/artificial-intelligence-medical-epidemiology-aime-1.
[11] “Sierra Leone In Action,” Global Health Security Agenda, https://www.ghsagenda.org/successes/sierra-leone-idsr-ghsa-in-action.
[12] Global Health Security Agenda, Implementing the Global Health Security Agenda: Progress and Impact from U.S. Government Investments (February 2018), https://www.ghsagenda.org/docs/default-source/default-document-library/global-health-security-agenda-2017-progress-and-impact-from-u-s-investments.pdf.
[13] “Assessment of Integrated Health Services for Key, Vulnerable and Migrant Populations at Cross-Border Sites in the East African Region, CB-HIPP/FHI 360” Source: FHI360. This assessment was presented at the Cross Border Health Integrated Partnership Project Baseline Evaluation and Lessons Learnt Validation Meeting but was not published separately.
[14] “Cross Border Health Integrated Partnership Project Baseline Evaluation and Lessons Learnt Validation Meeting Report (CB-HIPP unpublished, 2017).”Source: FHI360. This report was compiled based on the proceedings of the referenced meeting and made available to meeting participants, but has not been published separately.
[15] Broadband Commission for Sustainable Development, Digital Health: A Call for Government Leadership and Cooperation between ICT and Health (Geneva: February 2017), https://www.broadbandcommission.org/Documents/publications/WorkingGroupHealthReport-2017.pdf.
[16] “ICF Selected for $120 Million USAID Infectious Disease Detection and Surveillance Project,” CISION PR Newswire, July 30, 2018, https://www.prnewswire.com/news-releases/icf-selected-for-120-million-usaid-infectious-disease-detection-and-surveillance-project-300688549.html.
[17] “The Principles of Donor Alignment for Digital Health,” Digital Investment Principles, https://digitalinvestmentprinciples.org/.
[18] Jonathan Kourgialis, “Learning from Ebola: How Mobile Money can Prevent Health Crises,” Center for Financial Inclusion, August 15, 2018, https://www.centerforfinancialinclusion.org/learning-from-ebola-how-mobile-money-can-prevent-health-crises.
[19] Sherri Haas et al., Mobile Money for Health (Bethesda, MD: November 2013), https://www.hfgproject.org/wp-content/uploads/2013/12/Mobile-Money-for-Health-Case-Study.pdf.
[20] USAID, NetHope, and GBI, Information and Communications Technology Response to the Liberia Ebola Crisis: Desk Review and Recommendations for Private Sector Engagement (Fairfax, VA: October 24, 2014), https://solutionscenter.nethope.org/assets/collaterals/USAID_LiberiaICTDeskReview_Final_Nov414.pdf.
[21] Jeffrey Sturchio, “The Private Sector: A Partner in Global Health Security and Universal Health Coverage,” Rabin Martin, February 14, 2018, https://rabinmartin.com/insight/private-sector-partner-global-health-security-universal-health-coverage/.
[22] “A new Era in U.S. Development Finance,” OPIC, October 5, 2018, https://www.opic.gov/build-act/overview.
[23] “mDiabetes, an innovative programme to improve the health of people with diabetes in Senegal,” WHO, https://www.afro.who.int/news/mdiabetes-innovative-programme-improve-health-people-diabetes-senegal.
[24] “Coordinating Digital Transformation: Tanzania,” PATH/Digital Square, 2019, https://static1.squarespace.com/static/59bc3457ccc5c5890fe7cacd/t/5d07a3770c722300015fcbe7/1560781692272/Donor-Coord-Case-Studies_TANZ.pdf.